Prostate Cancer
Prostate Cancer is one of the most common cancers in males with over 19,000 men diagnosed each year in Australia. More than 3000 males die of Prostate Cancer each year in Australia.
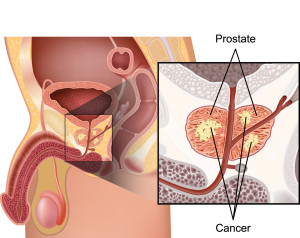
What is Prostate Cancer?
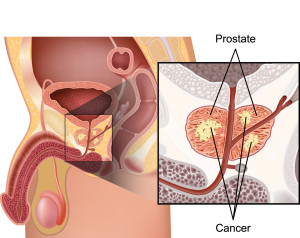
Prostate Cancer is when abnormal cells within the prostate develop and grow without control, and may spread outside the prostate to other parts of the body.
How dangerous is it?
Prostate cancer risk is divided into low, intermediate and high risk of spreading and developing into advanced disease and death. While many cases of Prostate Cancer are low risk and may never cause advanced disease in that man’s lifetime, higher risk disease can spread rapidly and needs appropriate treatment at as early a stage as possible.
What are the risk factors?
- Age – As age increases the risk of developing prostate cancer increases. The risk of developing prostate cancer is about 1 in 7 at age 70 and 1 in 5 at age 80.
- Family History – There is evidence that the the risk of prostate cancer is increased if a man has one or more first degree male relatives (father, brother, uncle) with the disease. This is especially so if the relative was diagnosed at a younger age (< 65). Males that carry the BRCA2 gene (which leads to breast and ovarian cancer in women) are at increased risk of prostate cancer.
What about lifestyle risk factors?
- Diet – Some evidence suggests that a diet high in processed meats and saturated fats can increase the risk of prostate cancer. A healthy diet should consist of a balance of foods from the five main groups in moderate portion sizes. See www.eatforhealth.gov.au for more information
- Exercise – A lack of exercise may contribute to cancer and other diseases. Spend at least 30 minutes a day doing some activity which increases your heart and breathing rate.
What are the symptoms of Prostate Cancer?
In the early stages, Prostate Cancer typically causes no symptoms. In the advanced stages it may cause:
- Urinary obstruction – poor urine flow
- Frequent urination
- Pain on urination
- Blood in the urine or semen
- Pain in the back, hips, pelvic bones or upper legs
How is it diagnosed?
- PSA – This blood test measures the level of PSA (prostate specific antigen) in the bloodstream and can help to diagnose prostate disease. PSA is made by the prostate and the level released into the blood can increases with Prostate Cancer. I may also be elevated with infection, trauma and benign enlargement of the prostate (BPH). PSA does not give a firm diagnosis of prostate cancer but allows the Urologist to judge whether a man is at high risk of Prostate cancer and needs further investigation, or if he is at very low risk and can be reassured.

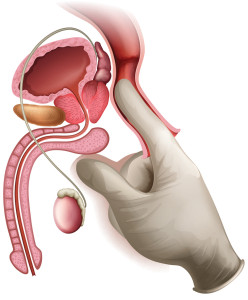
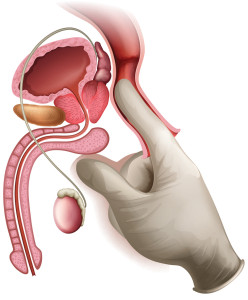
- DRE – Digital rectal examination. This simple and quick examination can yield important diagnostic information about the size and texture of the prostate. An abnormal DRE may be the only sign of prostate cancer before it causes symptoms. It is therefore an important part of any Urological examination in a male where prostate disease needs to be ruled out.
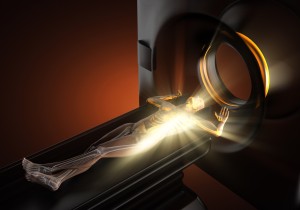
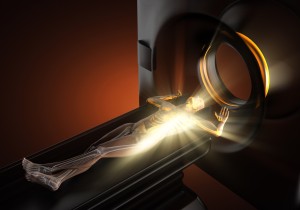
- MRI – The role of MRI for the investigation of prostate cancer has radically changed with the advent of multiparametric MRI (mpMRI) on newer, more powerful MRI machines (3T) .
The hope for mpMRI is to help address two of the problems in prostate cancer management: overtreatment and understaging ( an underestimation of the seriousness of the cancer).
Traditionally, men with a raised Prostate-specific antigen (PSA) level would be advised to have a prostate biopsy, which was the only way of deciding if there was any prostate cancer present.
On its own, the PSA blood test is not usually accurate enough to diagnose prostate cancer. Furthermore, the “standard” TRUS guided prostate biopsy techniques used may miss 10-20% of cancers, and sometimes underestimated the seriousness of the cancer. The reason for this is because TRUS guided biopsies are systematic biopsies designed to sample all areas of the prostate in a random fashion rather than targeting areas of cancer. Ultrasound and traditional lower powered MRI were just not accurate enough to be used to target abnormalitie
MpMRI scans the prostate in several different ways, giving slightly different information each time. When the results are combined, the radiologist can often see suspected areas of cancer which would otherwise not have been visible. This allows 3 significant benefits:
Using state of the art MRI guided in gantry biopsy (see below), we are able to very accurately target abnormal lesions thus increasing accuracy.
Potentially reducing the number of biopsises required hence reducing complications and side effects such as bleeding and infection.
There is increasing evidence that MpMRI is able to detect and distinguish between more aggressive prostate cancer as opposed to less aggressive types. This ability may help in reducing the risk of over treatment to pts.
-
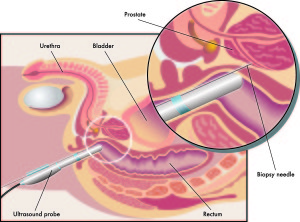
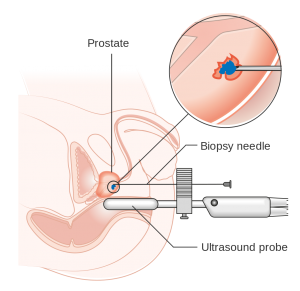
Prostate Biopsy – The only way Prostate Cancer can be definitively diagnosed is with a prostate biopsy. This is usually taken with a core biopsy needle either via a trans-rectal or trans-perineal route with ultrasound or MRI guidance. The trans-perineal route has a lower risk of serious infection, allowing more areas of the prostate to be biopsied in those who need it.
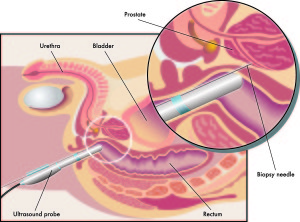
Trans-rectal Prostate Biopsy
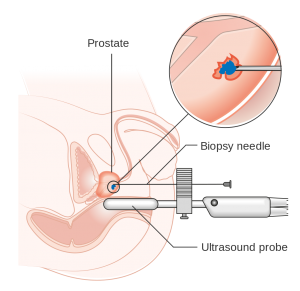
Trans-perineal Prostate Biopsy
How is Prostate Cancer Treated?
Localised Prostate Cancer: If prostate cancer is localised and has not spread, then several treatment options are available:
- Active Surveillance In some cases only small amount of low grade cancer is found. In such cases it is unlikely that the cancer will progress to spread outside the prostate for many years. It may be possible to monitor these cases with regular PSA checks, MRI and repeat biopsy. Some of these cases will develop into a more aggressive cancer and if there are signs that progression is developing, active treatment should be considered. active treatment consists of surgery or radiotherapy.
- Radical Prostatectomy This operation removes all of the prostate, and the seminal glands. In high risk cases, pelvic lymph nodes will also be removed. It is the best option for men who are otherwise healthy and can recover well from a reasonably large operation. The operation can be done in the following way:
Open Surgery – through an incision between the navel and the pubic bone.
Laparoscopic (keyhole surgery) with standard laparoscopic instruments inserted through small cuts in the abdomen and viewed with a high definition camera.
Robotic assisted Laparoscopy – With advanced surgical instruments using 3-D vision that makes the laparoscopic surgery easier to carry out with greater precision.
Laparoscopic and Robotic assisted surgery are both associated with shorter hospital stay, less bleeding and less pain than open surgery.
Link to Patient information for Robotic Assisted Laparoscopic Radical Prostatectomy:(RALP)
Benefits of Surgery:
The prostate is completely removed
Accurate staging and grading can be carried out.
PSA can accurately predict success of outcome
- Radiation Therapy Radiation therapy which aims to cure prostate cancer comes in 2 forms, external beam radiotherapy (EBRT) and Brachytherapy.Radiation therapy can be used as part of multimodal treatment for locally advanced prostate cancer after initial surgical removal of the prostate and the draining lymph nodes.Patients that require radiotherapy are referred to our colleagues at Genesis cancer care.
- Other therapies Treatments such as High intensity focused Ultrasound and Cryotherapy have inferior results to surgery and Radiotherapy and can be associated with greater complications. These treatments should only be carried out within the context of clinical trials.
Advanced Prostate Cancer
In advanced prostate cancer the tumour has spread outside the boundaries of the prostate and into adjacent tissue (locally advanced), or may have spread to a distant site (metastases) such as bone or lymph nodes.
In some locally advanced cases, there may still be a role for surgical removal as part of a multi-step approach with radiation therapy and hormonal therapy to follow if required.
In cases where there are distant metastases, the attention turns to controlling the cancer and slowing it’s growth.
- Hormone therapy Prostate cancer cells depend on testosterone (androgen hormones) for their growth. Certain medications can block the action of testosterone or decrease it’s production, thereby shrinking the tumour cells and stopping or slowing their growth. This can be effective for up to several years. Eventually the cancer cells will be able to grow without testosterone other types of therapy will need to be considered.
Injections which block testosterone production. These injections are given every 1-6 months as a slow release formulation.
Tablets to block the action of testosterone. These are anti-androgens and are taken orally on a daily basis or every second day.
Orchidectomy. Surgical removal of the testes (castration) will decrease testosterone levels to almost zero. There are still a small amount of androgen hormones produced by the adrenal glands. This form of hormonal therapy is irreversible.
Hormone therapy can cause side effects such as loss of libido, erectile difficulties, hot flushes, fatigue, weight gain, loss of muscle mass and strength, osteoporosis, heart disease, and worsening diabetes •
- Second line hormone therapy. Other combinations of hormonal therapies can be effective when the prostate cancer shows sign of progression despite initial hormonal treatment.
- Chemotherapy. Taxane-base chemotherapy has been shown to be effective against Prostate cancer in cases where the disease is no longer hormone sensitive.
- New Treatments. New treatments such as arbiraterone and enzalutamide attack the growth pathway of prostate cancer cells in different ways to hormonal therapy and have been shown to prolong survival in cases where the disease is resistant to hormonal therapy.