Microsurgical denervation of the spermatic cord, or ‘cord stripping’ is a procedure which can permanently treat chronic testicular pain in those who have exhausted all other options. Dr Barrett at Perth Urology Clinic has the largest experience with Microsurgical Denervation in Western Australia and is the first surgeon in Australia to perform the surgery robotically.
Chronic scrotal pain is a common condition that poses a unique set of challenges to the patient and the surgeon. There can be a physical cause within the scrotum or the pain can be a reflection of a disease process elsewhere (for example hip pain or back pain). Most commonly however the cause is not identified and this can lead to a frustrating impasse between patient and surgeon. Neuropathic pain can persist long after an initiating physical insult has healed.
Chronic pain should always be managed in a stepwise and multidisciplinary fashion with opinions from a pain specialist, physiotherapist and even a psychologist with a trial of all conservative options before surgery is considered. If a physical problem is identified (varicocele, post vasectomy congestion) then surgery can be offered to treat that problem.
Before the introduction of microsurgical denervation, urological surgery for pain would involve removal of the epididymus or the testicle. These operations were not ideal with low success rates and high complication rates.
The basis for the operation of microsurgical denervation is that the testicle is connected to the body through the spermatic cord. This can be thought of as a sheath of cables. Within this sheath (and amongst its ‘cables’) are the blood supply (arteries and veins), sperm drainage (vas deferens), muscle fibres and lymphatic channels. Intertwined amongst these vital structures are the nerves that carry sensation to and from the testicle. Regardless of the underlying cause of pain, the pain signals are presumed to be travelling through the spermatic cord and therefore disrupting this pathway can interrupt the pain signals. Patients who are suffering chronic scrotal pain have been shown to have nerves in the spermatic cord that are degenerative and abnormal.
The location of the degenerative nerves involved in chronic pain have been mapped out to three main locations within the spermatic cord. The majority of painful nerves are in the cremasteric fibres (the outer muscle sheath of the cord), around the vas deferens (the sperm carrying tube) and in the fatty tissue behind the cord. These areas are targeted and divided during denervation surgery. This targeted approach reduces the risk of any injury to the essential blood supply to the testicles.
Before proceeding with surgery, a local anaesthetic cord block temporarily blocks the pain signals within the cord and is a strong predictor of success with denervation surgery. If there is no response to a cord block, it is possible that the pain is coming from somewhere other than the testicle and other options should be considered. A cord block is required prior to a denervation and is performed in the rooms using a small needle under local anaesthetic. Pain scores will be recorded before and after the block.
The microsurgical denervation of the cord is performed through a small groin (subinguinal) incision. Through this incision the spermatic cord can be delivered.
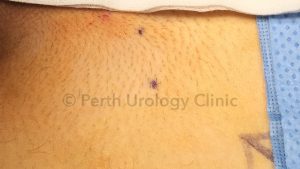



The cord is then opened under magnification using a microscope or a surgical robot and its contents can be examined. With meticulous care the targeted areas are divided while preserving the vas deferens and the essential blood vessels. The ilioinguinal nerve is ideally divided. At the end of the procedure the wound is closed with dissolving stitches after injection with local anaesthetic.
A patient will generally be discharged on the same day as surgery but on rare occasions may stay overnight. Activity needs to be limited for around 2 weeks.
The result of a successful denervation should be an improvement or resolution of scrotal pain. Because only the painful degenerative nerves have been cut the testicle itself should maintain some normal sensation but should have reduced sensitivity and reduced pain. There may be reduced sensation on a patch of skin on the scrotum and inner thigh if the ilioinguinal nerve is divided. There will be a patch of numb skin over the incision.
Worldwide series report excellent long term results in carefully selected patients undergoing microsurgical denervation. Approximately 80% of patients will have significant relief (a reduction in their pain scores by half or more) with approximately 50% of patients reporting a resolution of their pain.
There are some potential risks related to the procedure such as damage to the testicle, loss of the testicle and hydrocele formation but these are thankfully very rare.