Painful Bladder Syndrome

Painful Bladder Syndrome/Interstitial Cystitis (PBS/IC)
People with Painful bladder Syndrome/Interstitial Cystitis (PBS/IC) suffer pain when the bladder is full and/or have to urinate frequently. The cause is unknown. Diagnosis is based around excluding all other causes of pain (from stones, infection etc). Unfortunately there is no conclusive test to prove someone has interstitial cystitis.
Nine out of ten sufferers are women. It can develop at any age, with the onset for most patients around the age of 40 years. Many women are diagnosed in their 30s.
PBS/IC is a chronic, debilitating syndrome and people respond variably to treatment. There is no cure, but patients may achieve long remissions.
What are the symptoms of painful bladder syndrome interstitial cystitis (PBS/IC)?
- Pain. The main symptom is pain when the bladder is full, with a feeling of some relief on voiding, or emptying, the bladder. Pain may be felt in the pelvis, abdomen and in the vagina. Pain may be worse with bladder filling, voiding or during sexual intercourse. Men may feel pain in their prostate, scrotum or penis.
- Frequency. Having to urinate frequently, including overnight, is a classic sign of IC. People with the condition may urinate 40 or 50 times in 24 hours in most severe cases compared to the usual seven or eight.
- Urgency may also develop. This means a person is unable to delay urination and they may feel an urge to urinate even immediately after doing so. It is usually associated with urinary leakage or a fear of leakage. Some describe a constant desire to pass urine.
What causes of painful bladder syndrome interstitial cystitis (PBS/IC)
The cause of PBS/IC is unknown but several theories are being investigated.
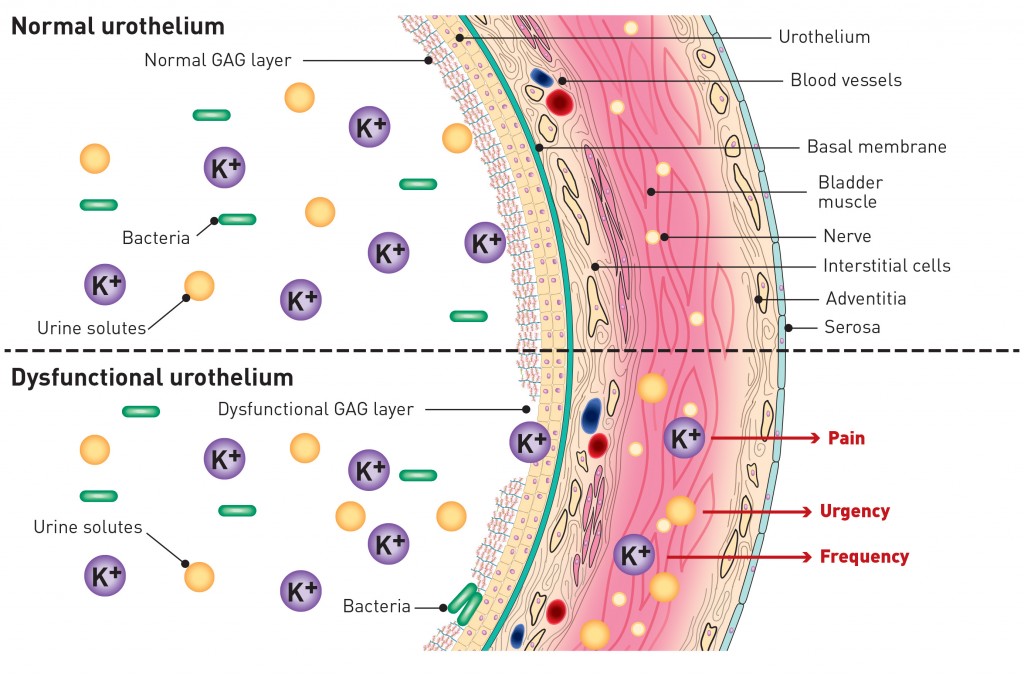
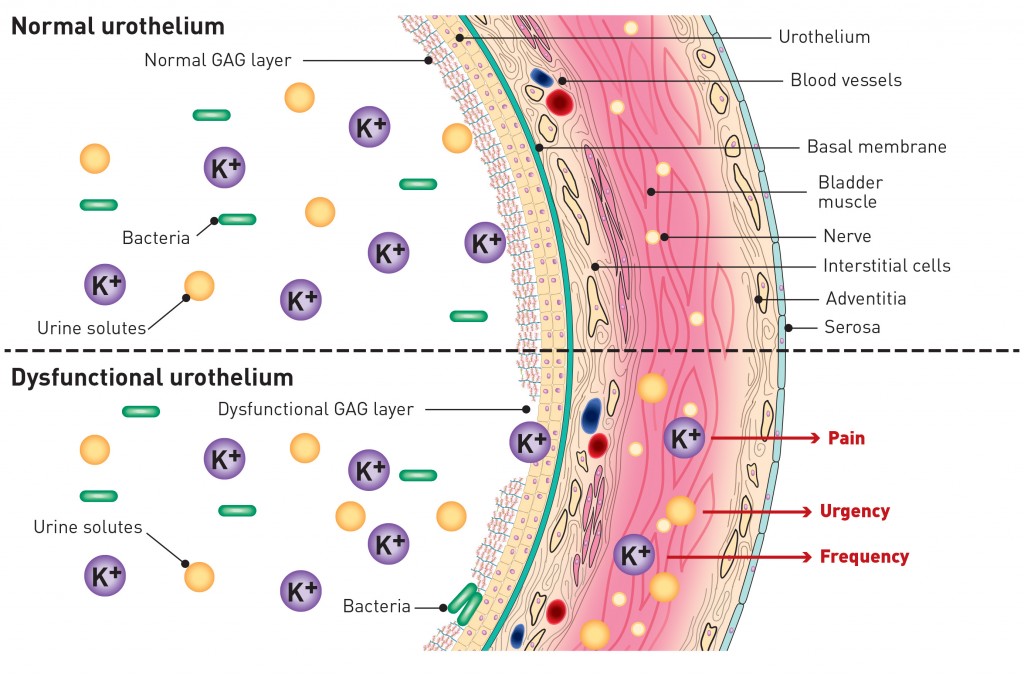
- Leaky bladder lining – The bladder is lined with a layer of glycosaminoglycans (GAG) which protect it from irritation. PBS/IC might be caused by a defect in part of this lining of the bladder, the so-called GAG layer. In a healthy bladder this is a natural barrier that protects the bladder lining from irritating and toxic substances found in urine, however if this barrier is damaged, urine comes into direct contact with the tissues of the bladder lining and over time can cause damage to these tissues, as well as allowing bacteria to adhere.
- Histamines. PBS/IC symptoms may be caused by an allergic reaction leading to the release of histamines from cells (known as mast cells) in the bladder wall. The histamines cause swelling and inflammation of the bladder lining.
- Autoimmune response. The body s immune system may attack the bladder. PBS/IC is more common in women with autoimmune conditions.
- Irritating urine. It may be that there is an agent in the urine of sufferers which inflames the bladder.
- Post-surgical condition. PBS/IC is known to occur after hysterectomy but the reasons why are not clear.
- Infection. PBS/IC might be caused by an as yet undiscovered trigger, such as a viral infection.
How is PBS/IC diagnosed?
No simple test diagnoses PBS/IC. Your specialist needs to take a medical history, perform a physical examination, and suggest several investigations to rule out other conditions such as overactive bladder, endometriosis, infection, and cancer.
- A urine sample will be tested to check for infection. Usually it is found to be normal in people with PBS/IC
- Cystoscopy (a telescope introduced to the bladder through the urethra) is a useful test to rule out many other irritating conditions of the bladder. Most of the time, the bladder lining looks normal but rarely a red patch may be seen (Hunners ulcer) which suggests the presence of PBS/IC. If a Hunners ulcer is seen, resecting or burning it may relieve symptoms.
- Hydro-distension, which is the filling of the bladder during cystoscopy may demonstrate Hunners ulcers and may itself relive symptoms.
- Bladder Biopsies may be taken to exclude other diseases including malignancy.
How is PBS/IC treated?
A range of treatments may be tried before a patient achieves remission. These treatments are usually offered in a step-by-step process to see what works for each individual.
- Physical therapy
- Physical therapy with a sub specialised physiotherapist is the first step in learning how to mediate your bodies reaction to pain and work on strategies to control it
- GAG layer replacement therapy
- This is a new and exciting therapy specifically designed to repair the damage to the GAG layer and so restore the bladder’s protective coating.
- It treatment begins with a course of instillations given once a week for the first month, and then once every two weeks for the second month. After this, instillations are given once every month until symptoms settle down.
- More information may be found at this link.
- Other bladder instillations
- Dimethyl sulfoxide or DMSO (Rimso-50), a chemical solvent from wood pulp which has several uses in medicine. It is known to reduce inflammation and block pain in about a third of IC patients. It is a potent destroyer of free radicals that damage cells. It has the rather bizarre side-effect of leaving patients smelling of garlic.
- Heparin, an anti-coagulant which is sometimes mixed with DMSO.
- Steroids mixed with DMSO
- Oral drugs
- Amitriptyline, an antidepressant used to block pain. This drug has sedating and anti- cholinergic (suppression of urge to urinate) effects.
- Gabapentin, a pain modifier.
- Anti-histamines, believed to reduce inflammation in the bladder.
- Pentosan polysulfate (Elmiron), a drug approved for IC and designed to help restore the GAG layer of the bladder wall. This is not on the PBS and costs about $200 per month. Side-effects include gastrointestinal upset and liver dysfunction.
- Surgery
- When all else fails, and particularly when the patient has a progressive condition where they are losing bladder volume, surgery can be considered. Types of surgery:
- Hydro-distension (filling the bladder with saline while under anaesthetic) is often undertaken as part of diagnosis but can also relieve symptoms in about half of patients. Weeks or even months of relief may follow, and the procedure can be repeated if successful.
- Sacral neuromodulation. Electrodes are implanted in the lower back which block nerves that transmit pain from the bladder. This procedure should be carried out in specialist centres.
- Botox. Injections of botox into the bladder may help with pain.
- Urinary diversion (ileal conduit). This operation allows urine to by-pass the bladder and be collected in a bag on the outside of the abdominal wall. Despite the body image issues created by this option, many patients value the freedom it gives them because they do not have to worry about proximity to a toilet. Over time some people who have had this operation may suffer deterioration of their kidneys.
- Bladder removal (cystectomy). Very occasionally, when pain persists despite urinary diversion, the bladder may be removed. Even still pain can persist.
What else can I do?
- Modify diet. Some foods and drinks are known to make symptoms worse in many patients. These include tomatoes, citrus fruits, bananas, chocolate, cheese, mayonnaise, nuts, onions, raisins, sour cream, yoghurt, spicy foods, coffee, wine, beer and carbonated drinks. Patient support groups are often a good source of information about bothersome foods. Not everyone will be affected the same way so many people try an elimination diet, cutting out suspect foods one by one to see which may cause symptoms.
- Look after yourself. Living with interstitial cystitis can cause significant stress and psychological effects. Constant sleep deprivation because you have to get up and go to the toilet impacts severely on a patients well-being. Patients may feel tied to the toilet and unable to have a normal life, which also affects their mental health. The stigma associated with this kind of condition, coupled with chronic pain, can wear people down. Anti-depressants prescribed as a pain moderator may also help improve a patient s psychological state. Joining a support group (see above) can help too.
What is my longterm prognosis?
Most commonly, patients will have symptoms grumbling on and off for years. They will undergo a treatment, achieve remission, then find that symptoms return and may have to try something else. PBS/IC is a condition that tends to recur.
A smaller group of patients will progressively lose bladder volume as despite treatment, progressive scarring of the bladder wall occurs, so not only does pain persist, but bladder volume reduces. These patients are often candidates for urinary diversion surgery.
A third group of patients appears to fulfil the diagnostic criteria for PBS/IC at first but recovers completely. Urologists believe that if the condition becomes cured it probably was not PBS/IC in the first place.
What is my first step in managing my bladder pain?
Make an appointment with one of our clinicians.
We have a group that is focussed on taking a multidisciplinary approach to pelvic pain and although it can be a very difficult condition to treat, we can set you on the right path.
This information has been adapted from the fact sheet produced by the Female Urology Special Advisory Group (SAG) of the Urological Society of Australia and New Zealand
Here is another downloadable information sheet NIDDK Interstitial Cystitis